How a large national health plan leveraged integrated capabilities to increase Medicaid enrollment by over 17%.
Embel Assist implements solutions that turn disconnected engagement into whole-person conversations.
Powered by real-time data, automation, and a tech-neutral approach, we help organizations orchestrate communication across every stage of a person’s health journey.










Healthcare isn’t failing because of a lack of investment or effort. It’s strained by fragmentation and complexity, optimized for transactions instead of people. The result is predictable: confusion, disengagement, and care experiences that feel impersonal.
Embel Assist serves as a guided partner and advisor to health plans, health systems, and self-insured employers. We bring clarity and structure to how organizations communicate, helping teams deliver the right message at the right time across every stage of health.
Real progress comes from intentional choices. We work alongside teams ready to make them.
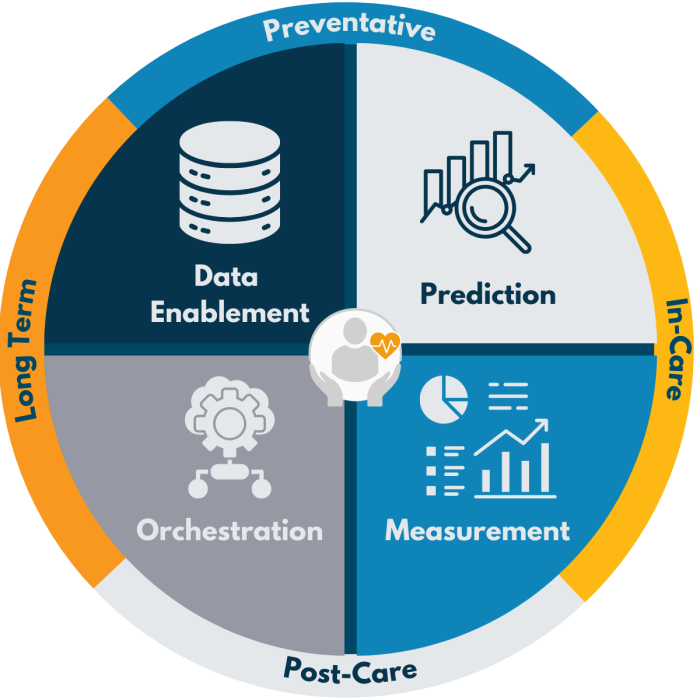
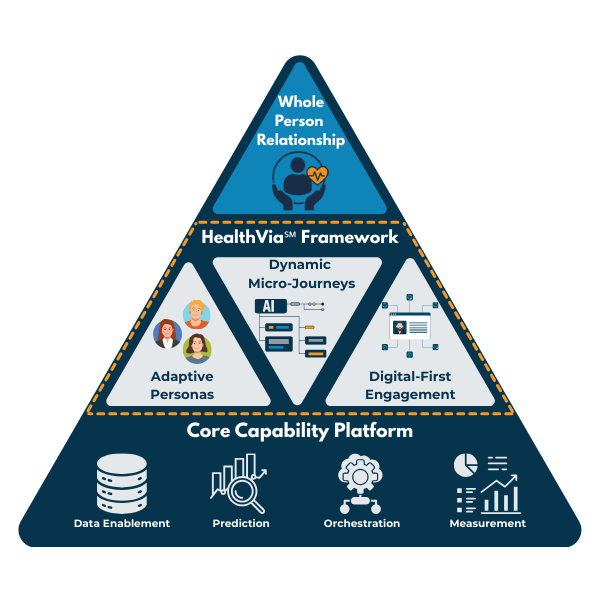
HealthVia℠ is a whole-person communication framework that helps organizations engage people with greater intention and relevance. By combining dynamic personas, tailored journeys, and digital-first outreach, it guides who to reach, when to engage, and what comes next.
The result is fewer gaps in care, less operational strain, and stronger connections between individuals and the teams supporting their health.
Data-driven insights identify risks early, enabling proactive, personalized outreach—like catching heart disease risks in individuals who skip check-ups.
Predictive models trigger timely actions, like scheduling post-op follow-ups to prevent complications. Automated outreach across portals, apps, EHRs, and SMS closes care gaps.
Automated messaging keeps individuals engaged with reminders and check-ins on their preferred channels—ensuring ongoing support without unnecessary office visits.
Smart reminders and behavioral insights make adherence effortless—like voice alerts helping elderly populations stay on track with medications.
Automated workflows sync interactions across touchpoints, ensuring seamless, personalized engagement at every stage of their health journey.
Data-driven strategies identify engagement gaps and health disparities, enabling targeted outreach that improves access, equity, and STAR performance.
Discover how prepared you are to deliver exceptional health outcomes. Take our Health Engagement Maturity Index assessment to evaluate your strategies, capabilities, processes, and organizational alignment for a total consumer experience. It’s free, no strings attached…give it try and start using your score to drive change today.
How a large national health plan leveraged integrated capabilities to increase Medicaid enrollment by over 17%.