“They provided not only the technical expertise in developing the reports but were able to work with our internal stakeholders in understanding our needs and guide us down the right path”
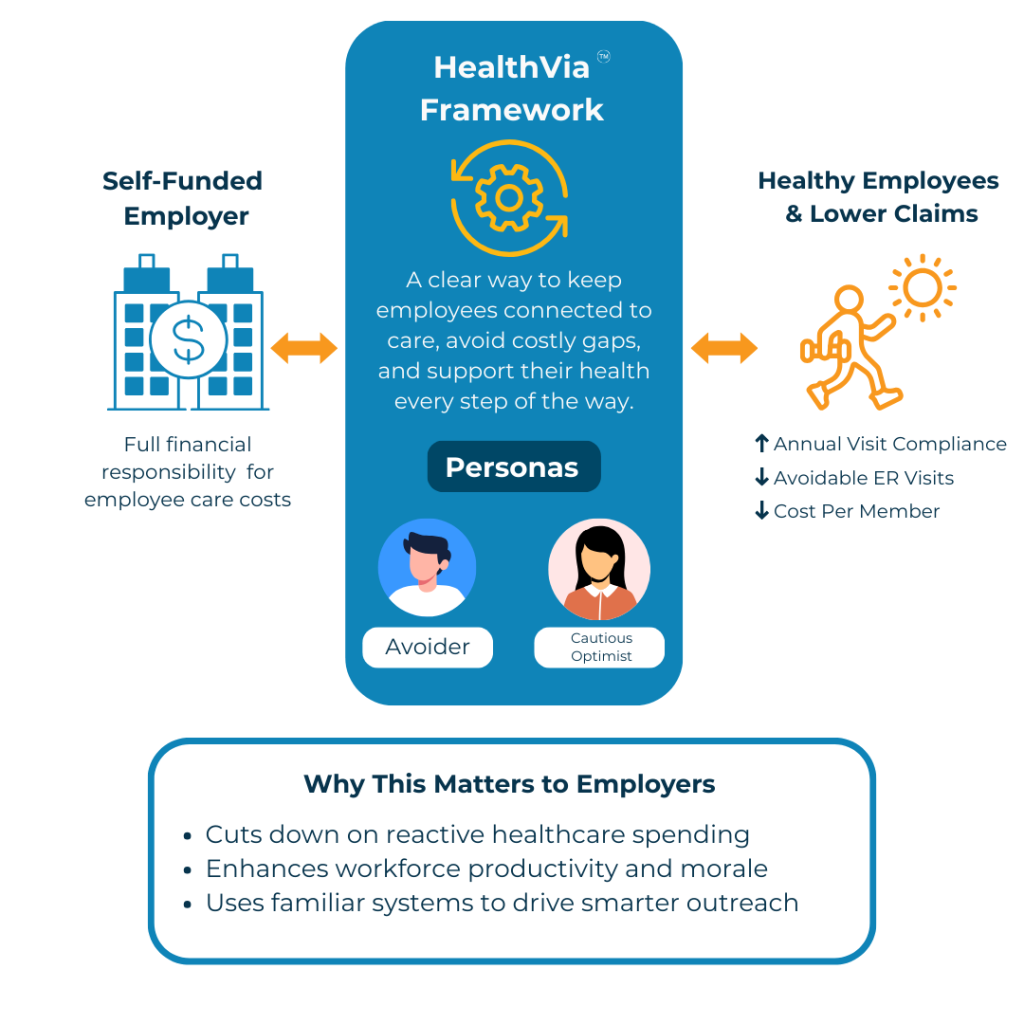
Helping employers reduce costs, improve engagement, and enhance health plan outcomes.