“They take the time to understand the company needs, processes, the workstyles and helped to identify how we can incorporate technology to achieve our process goals”
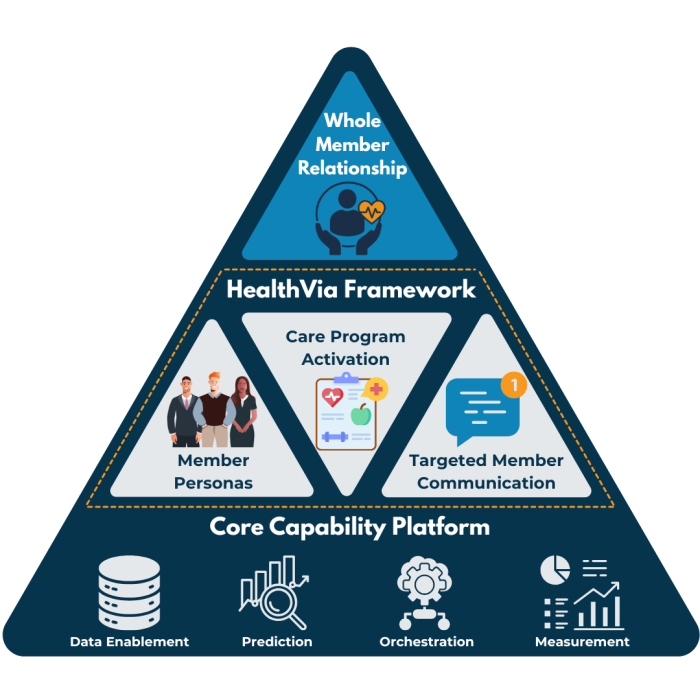
We help payers design and deliver personalized digital-first engagement that guides members through every stage of their health journey. From onboarding and prevention to chronic care and recovery, we combine intelligent automation, compassionate communication, and data-driven insights to improve outcomes and increase member satisfaction.