“I would recommend Embel Assist to any organization that needs subject matter experts in marketing execution and consumer engagement”
Improve member outcomes, reduce costs, and boost operational efficiency with data-driven strategies.

Improve member outcomes, reduce costs, and boost operational efficiency with data-driven strategies.
• Identify high-risk members early to implement preventive strategies and reduce costs.
• Use data analytics to track health trends and improve decision-making across programs.
• Optimize care coordination to ensure members receive timely and effective interventions.
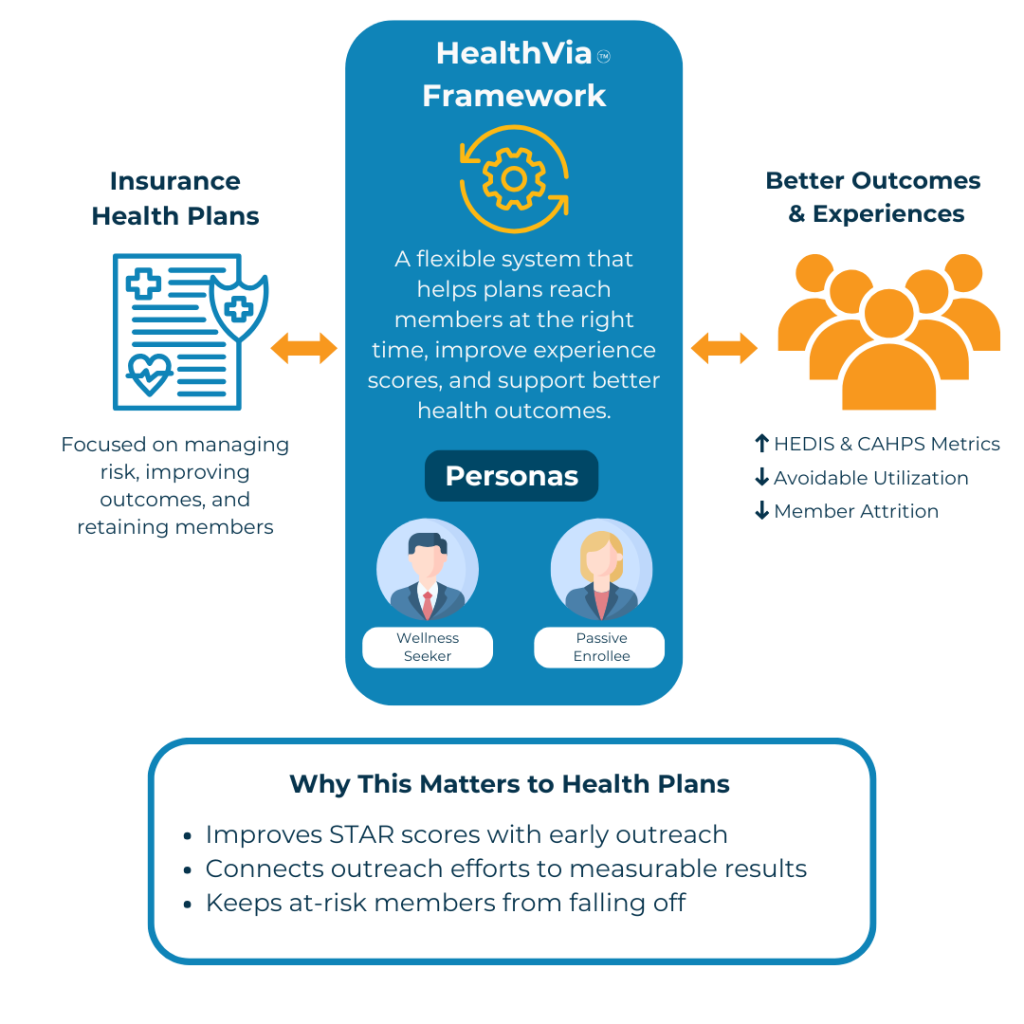
• Develop health personas to design customized benefits based on member needs.
• Use digital tools to enhance program accessibility and drive member engagement.
• Offer personalized outreach that promotes active participation in health improvement.
• Integrate care management systems for real-time tracking and better care coordination.
• Enable seamless communication between care teams and patients, reducing gaps in care.
• Align member care pathways to avoid duplications and reduce unnecessary interventions.
• Predict and manage high-cost claims by identifying risk factors early in the process.
• Create tailored interventions for high-risk members to reduce future healthcare expenses.
• Collaborate with healthcare providers to implement risk-reduction programs effectively.
How a large national health plan leveraged integrated capabilities to increase Medicaid enrollment by over 17%.
Discover how a regional care delivery organization revolutionized patient engagement to achieve ambitious goals over the next 3 years.
How a large national health services organization increased program enrollment by over 200%.