“Embel Assist has proven to be a trusted and cost effective partner to help us better leverage our campaign management investments”
Equip care teams to deliver precise, scalable outreach that connects patients and drives outcomes.

Equip care teams to deliver precise, scalable outreach that connects patients and drives outcomes.
HealthVia℠ helps self-funded employers reduce avoidable claims, guide smarter choices, and improve employee outcomes while minimizing internal lift.
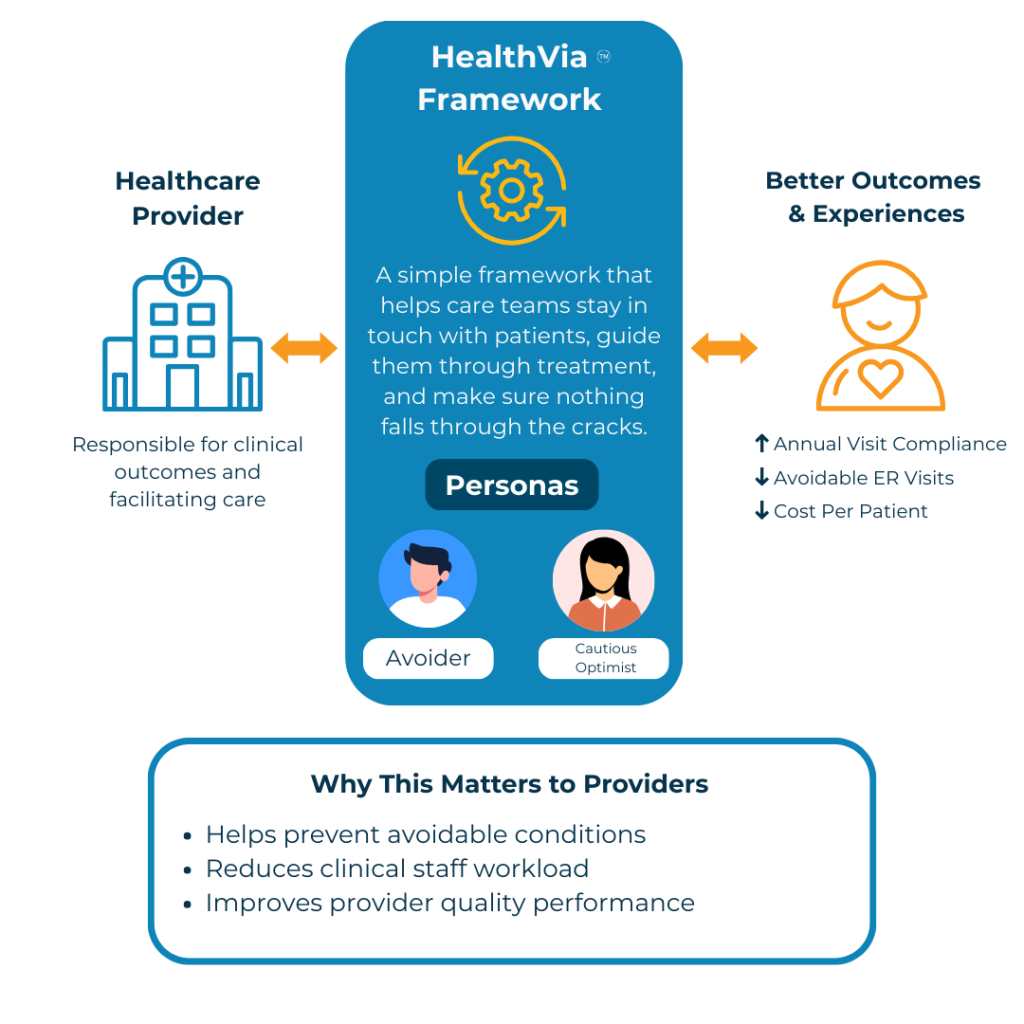
Proactive, digital-first outreach ensures patients receive the right information, support, and next-best actions—whether in prevention, active care, or post-care recovery.
How a large national health plan leveraged integrated capabilities to increase Medicaid enrollment by over 17%.
Discover how a regional care delivery organization revolutionized patient engagement to achieve ambitious goals over the next 3 years.
How a large national health services organization increased program enrollment by over 200%.